WINNIPEG -- A recent report shows access and affordability is different for arthritis drugs depending on where you live in Canada.
The report gives a lay of the land on current arthritis drug availability in the country, and shows where a national drug plan could help with inequities in the system.
"That's disparities for people on private plans and on public plans," said Joanne Di Nardo, the director of public policy & government affairs for the Arthritis Society.
The research was done by The Conference Board of Canada and funded by the Arthritis Society.
The report says a national pharmacare model could ensure all Canadians can access and afford the drugs they need. It would need to include biologics, which are innovative drugs made from living organisms used in arthritis treatment. Di Nardo said it's also important patients have a say in what a national plan would look like.
"So that we understand who is going to be utilizing the plan, and how they are going to be utilizing it so that it's not limiting and we don't have people who have undue financial burden," she said.
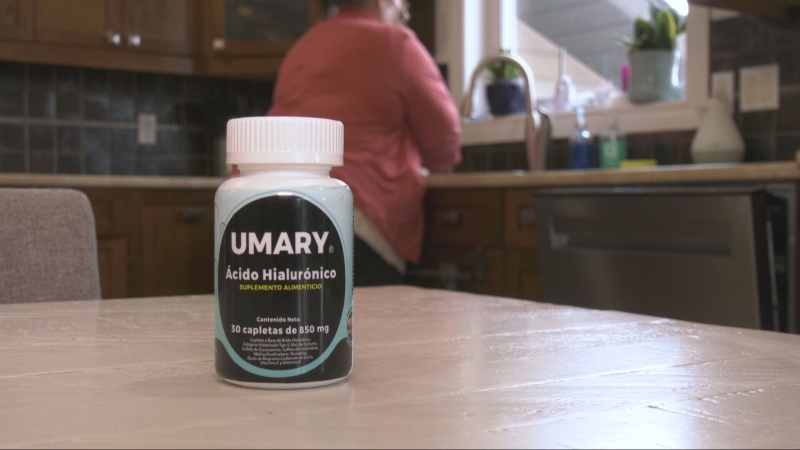
Darlene Mcpherson has been living with rheumatoid arthritis for 30 years.
The former teacher told CTV news a more simplified system for drug coverage would help her quality of life.
"I have to go through a lot of hoops to get some benefits," Mcpherson explained. "Wouldn't it just be so nice if I could just go to the pharmacy and pick up my medication so that I could at least contribute something."
The biologic drug she is on costs her $1,600 a month. She does have a mix of public and private drug coverage in order to afford it, she also said the drug company helps out based on her income.
A spokesperson from Manitoba Health told CTV News it introduced a tiered-biologic framework in 2018 that aligns with the pan-Canadian Pharmaceutical Alliance’s first principles.
“The first tier ensures coverage for biologics or biosimilars that are determined to be the most cost-effective, or for biologics that have successfully negotiated an agreement through the pan-Canadian Pharmaceutical Alliance,” read a written statement. “The second tier ensures coverage for biologics that have an expired agreement/no agreement if clinical need is demonstrated.”
The full report from The Conference Board of Canada can be found here.