What the COVID-19 pandemic has revealed about Manitoba's health-care system
Two years into the COVID-19 pandemic, Manitoba has gone trough a journey with unprecedented challenges.
Since the start of the pandemic, Manitoba has reported more than 130,000 cases of COVID-19 and more than 1,700 deaths.
These statistics measure a two-year-long pandemic that's hit health care in the province hard.
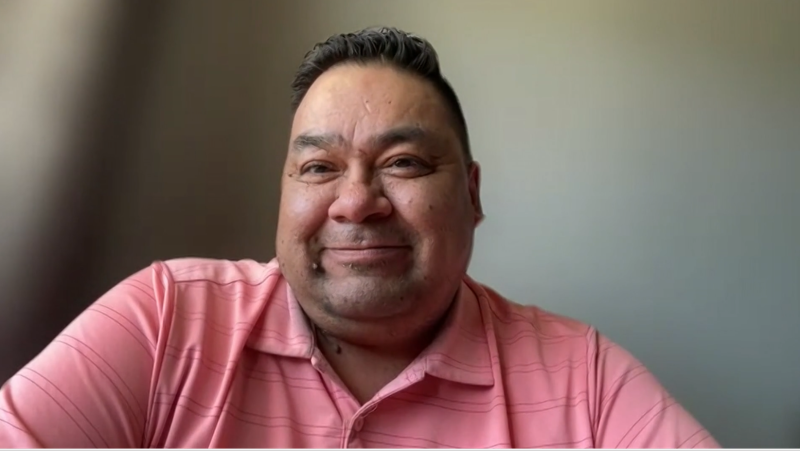
"One thing this pandemic has shown us is how tenuous our health-care system is," said Dr. Kristjan Thompson, president of Doctors Manitoba,
According to Dr. Philippe Lagace-Wiens, a medical microbiologist, the system was not ready for the back-to-back waves or surges of patients needing hospital care
"Our health-care system has been designed over years and years and through consultation processes to try and get it so refined that it works at 95 to 98 per cent capacity all the time, so it can’t even really respond to a bad influenza season let alone a global pandemic," said Lagace-Wiens.
He said increasing capacity requires investment.
“You have to accept that there is going to be some extra cost that isn’t necessarily utilized at 98 per cent,” he said.
Dr. Bob Bell, former Ontario deputy minister of health and long-term care, said the surge capacity issue isn't isolated to Manitoba.
His idea is to build intermediate or transitional-care centres into the system to free up hospital space and resources.
“It's less expensive than hospitals. We don’t have to worry about the labs. We don’t have to worry about the ORs. We don’t need the same skill mix of all RN staff that we often see in hospital units,” Bell said
Darlene Jackson, president of the Manitoba Nurses Union, said what's also needed are ways to keep the physicians, nurses and homecare staff we have in the province, because training new people is a long-term solution.
"We're in a global nursing shortage, and for sure a national one, so other provinces are actively vying to hire nurses away from us,” Jackson said.
At the same time, virologist Jason Kindrachuk said other important lessons learned are the airborne transmission of COVID-19, and measuring the spread through wastewater.
"We have to take those out of Covid and move those forward for other emerging viruses because, listen, this is not the last pandemic and certainly not the last emerging virus we are going to see,” Kindrachuk said.
As for transitional beds, a Shared Health spokesperson says there are 279 in the province.
The spokesperson said the beds generally serve patients with fewer needs for a limited amount of time before being they are sent home or to a long-term care facility.
CTVNews.ca Top Stories

BREAKING New York appeals court overturns Harvey Weinstein's 2020 rape conviction from landmark #MeToo trial
New York’s highest court on Thursday overturned Harvey Weinstein’s 2020 rape conviction, finding the judge at the landmark #MeToo trial prejudiced the ex-movie mogul with improper rulings, including a decision to let women testify about allegations that weren’t part of the case.
BREAKING Monthly earnings rise, payroll employment falls: jobs report
The number of vacant jobs in Canada increased in February, while monthly payroll employment decreased in food services, manufacturing, and retail trade, among other sectors.
Doctors say capital gains tax changes will jeopardize their retirement. Is that true?
The Canadian Medical Association asserts the Liberals' proposed changes to capital gains taxation will put doctors' retirement savings in jeopardy, but some financial experts insist incorporated professionals are not as doomed as they say they are.
Remains from a mother-daughter cold case were found nearly 24 years later, after a deathbed confession from the suspect
A West Virginia father is getting some sense of closure after authorities found the remains of his young daughter and her mother following a deathbed confession from the man believed to have fatally shot them nearly two decades ago.
Something in the water? Canadian family latest to spot elusive 'Loch Ness Monster'
For centuries, people have wondered what, if anything, might be lurking beneath the surface of Loch Ness in Scotland. When Canadian couple Parry Malm and Shannon Wiseman visited the Scottish highlands earlier this month with their two children, they didn’t expect to become part of the mystery.
Metro Vancouver mayors call for serial killer Robert Pickton to be denied parole
A dozen mayors from around Metro Vancouver say federal Attorney General and Justice Minister Arif Virani should deny parole for notorious B.C. serial killer Robert Pickton, and reassess the parole and sentencing system for 'prolific offenders and mass murderers.'
What do weight loss drugs mean for a diet industry built on eating less and exercising more?
Recent injected drugs like Wegovy and its predecessor, the diabetes medication Ozempic, are reshaping the health and fitness industries.
2 military horses that broke free and ran loose across London are in serious condition
Two military horses that bolted and ran miles through the streets of London after being spooked by construction noise and tossing their riders were in a serious condition and required operations, a British government official said Thursday.
'It was instant karma': Viral video captures failed theft attempt in Nanaimo, B.C.
Mounties in Nanaimo, B.C., say two late-night revellers are lucky their allegedly drunken antics weren't reported to police after security cameras captured the men trying to steal a heavy sign from a downtown business.