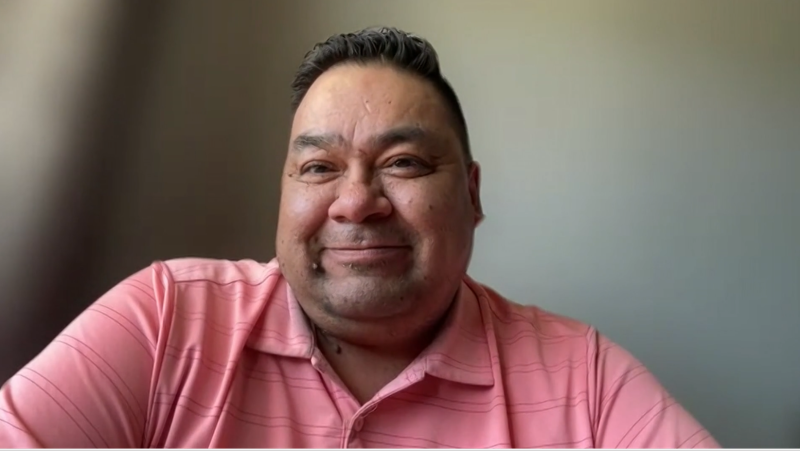
New data shows the impact of the pandemic's third wave on Manitoba's BIPOC community
As the COVID-19 pandemic slows in Manitoba, provincial medical leaders are already looking at data that shows systemic issues put people who aren’t white at a higher risk of hospitalization.
The data also shows that during the third wave of the pandemic, the proportion of cases of people identifying as white has gone down, while cases among BIPOC (Black, Indigenous and People of Colour) communities have increased.
"The gap in cases between all BIPOC communities combined and cases who identified as white has grown since December," Dr. Marcia Anderson said on Monday.
Dr. Anderson, the Pandemic Response Coordination Team’s medical lead, presented the province’s third wave Race, Ethnicity, Indigenous (REI) Analysis at Monday’s COVID-19 news conference.
Between March 31st and June 7th, nearly 77 per cent of the 18,808 COVID-19 cases were asked about their racial, ethnic, or Indigenous identity. A small percentage declined to answer the question.
Notably, nearly 17 per cent of cases were reported among Indigenous communities, as well as 10.5 per cent and 10.3 percent among South Asian and Southeast Asian populations, respectively.
White communities accounted for over 35 per cent of COVID-19 cases during the time.
The data show the age-standardized rate of COVID-19 infection among BIPOC communities is more than 21 times higher compared to white communities and hospitalization rates were 3.5 times higher – and four times higher in ICU admissions.
People identifying as Chinese were the only population group underrepresented among COVID-19 numbers, though Dr. Anderson noted they’ve experienced other negative impacts related to the pandemic – specifically related to a rise in anti-Asian hate crimes.
A population group labelled ‘Others’ accounted for approximately 8.5 per cent of cases. The most common responses among this group were multiracial people and those identifying as Middle Eastern or a related ethnicity.
Dr. Anderson said the diverse rates among BIPOC communities could be related to differences in housing and income status, occupational risks, or underlying conditions.
She said the effects on diverse communities include stress for members in isolation, in hospital, or those grieving deaths caused by COVID-19. She added these effects increased delays on access to vaccinations among these groups.
Anderson said BIPOC community members have, “felt stigmatized by messages that people in hospital died something wrong,” by not following public health orders or failing to get vaccinated.
The analysis states vaccination efforts and resources should utilize community partnerships and concentrate on areas where rates are the lowest. However, it also notes vaccinations alone aren’t sufficient in addressing gaps in health care, and planning for the fourth wave needs to prioritize addressing these barriers.
LATER VACCINATIONS FOR BIPOC COMMUNITIES
The data also showed high-risk people from BIPOC communities in Manitoba were vaccinated too late to prevent many hospitalizations.
For the most part, Manitoba used an aged-based approach for eligibility in its COVID-19 vaccine rollout.
The report compared the average age of white Manitobans who were hospitalized due to COVID-19 (60 years) to the average age of BIPOC Manitobans hospitalized with the virus (46 years) from March 31, 2021 to June 7, 2021.
The 14-year difference meant "the average person from a BIPOC community admitted to hospital wasn’t eligible for the vaccine until 23 days later than the average white person admitted to hospital," according to the report.
“The majority of those hospitalizations could have been prevented if people were able to get vaccinated on the same day that they were eligible," Anderson said.
Dr. Brent Roussin, Manitoba’s chief provincial public heath officer said early on in the pandemic, vaccine supply was the most limiting factor for the vaccine rollout.
“The most dramatic risk factor was age, and that was how things were rolled out at first, as we saw more and more risk factors, have gotten more and more vaccine in, and then we're able to do some more of those targeted interventions,” said Dr. Roussin.
On April 23, 2021 the province started the neighbourhood-based approach and on April 26, 2021, the Urban Indigenous clinics opened.
When asked why other strategies were not tried earlier, Dr. Roussin said the planning a vaccine rollout is complex.
“I think we like anytime we implement these things we learn lessons from it,” Dr. Roussin said.
CTVNews.ca Top Stories

BREAKING Honda to get up to $5B in govt help for EV battery, assembly plants
Honda is set to build an electric vehicle battery plant next to its Alliston, Ont., assembly plant, which it is retooling to produce fully electric vehicles, all part of a $15-billion project that is expected to include up to $5 billion in public money.
BREAKING Appeals court overturns Harvey Weinstein's 2020 rape conviction from landmark trial
New York’s highest court on Thursday overturned Harvey Weinstein’s 2020 rape conviction, finding the judge at the landmark #MeToo trial prejudiced the ex-movie mogul with improper rulings, including a decision to let women testify about allegations that weren’t part of the case.
1 arrested in northern Alberta during public shelter order
Residents of John D'Or Prairie, a community on the Little Red River Cree Nation in northern Alberta, were told to take shelter Thursday morning during a police operation.
Secret $70M Lotto Max winners break their silence
During a special winner celebration near their hometown, Doug and Enid shared the story of how they discovered they were holding a Lotto Max ticket worth $70 million and how they kept this huge secret for so long.
Remains from a mother-daughter cold case were found nearly 24 years later, after a deathbed confession from the suspect
A West Virginia father is getting some sense of closure after authorities found the remains of his young daughter and her mother following a deathbed confession from the man believed to have fatally shot them nearly two decades ago.
Monthly earnings rise, payroll employment falls: jobs report
The number of vacant jobs in Canada increased in February, while monthly payroll employment decreased in food services, manufacturing, and retail trade, among other sectors.
First in Canada procedure performed at London, Ont. hospital
A London man has become the first person in Canada to receive a robotic assisted surgery on his spine. Dave Myeh suffered from debilitating, chronic back pain that led to sciatica in his right now and extreme pain in his lower back.
Doctors say capital gains tax changes will jeopardize their retirement. Is that true?
The Canadian Medical Association asserts the Liberals' proposed changes to capital gains taxation will put doctors' retirement savings in jeopardy, but some financial experts insist incorporated professionals are not as doomed as they say they are.
Something in the water? Canadian family latest to spot elusive 'Loch Ness Monster'
For centuries, people have wondered what, if anything, might be lurking beneath the surface of Loch Ness in Scotland. When Canadian couple Parry Malm and Shannon Wiseman visited the Scottish highlands earlier this month with their two children, they didn’t expect to become part of the mystery.