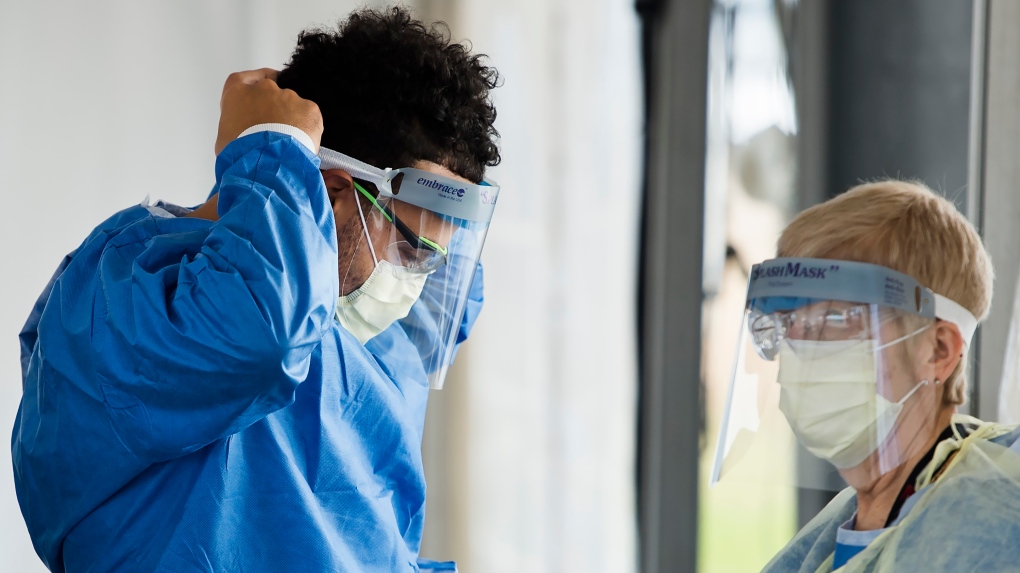
WINNIPEG -- With Manitoba recording dozens of new COVID cases each day recently - anxiety has been building among healthcare workers on the front lines.
Labour leaders in the province say they are hearing of rising concerns about staffing levels, time off, and flex in the system.
“As the numbers increase, the anxiety levels increase,” said Debbie Boissonneault. She is the president of CUPE 204 which represents 14,000 healthcare support workers in Manitoba at about 60 different sites.
She explained that in recent weeks her membership working in hospitals, long-term care homes and clinics have many questions about the second wave.
“Why are people still allowed to come into visit loved ones when the numbers keep going up?” she said. “There’s questions about having people go out from personal care homes and coming back and not being isolated into a room where they could possibly have come into contact with someone with COVID.”
The once flat curve in Manitoba is trending up, with 32 new cases Wednesday and three additional deaths.
“Second place in the country is not where we want to be right now,” said MGEU President Michelle Gawronsky who said she is hearing about burnout and fear of infection from her membership on the front lines.
MGEU represents 10,000 healthcare workers in Manitoba. That includes staff at Selkirk mental hospital, Cadham provincial lab, the addictions foundation of Manitoba, healthcare aides in personal care homes and hospitals, home care attendants and paramedics in Winnipeg.
Gawronsky said it’s time to put the people first.
“Make sure all positions are filled, that they have exhausted all possibilities of having back up staff having people readily available to be able to replace them, making sure the facilities are there as they are needed,” she told CTV news.
Filling vacancies is also a concern of the Manitoba Nurses Union.
“Nurses are absolutely working flat out,” said MNU President Darlene Jackson.
Jackson said Manitoba went into the pandemic with a nursing shortage, including positions in the intensive care unit.
Now that Manitoba is in the second wave, Jackson wants to know when a similar action to the first wave will happen, like surgery cancellations, the opening of additional beds, or reduced visitation.
“There needs to be a plan in place,” Jackson said, “there needs to be some type of plan on how we are going to manage a spike."
Bob Moroz, president of Manitoba Association of Health Care Professionals, wrote of similar concerns from his members in a statement to CTV news.
“Of course there is heightened concern as COVID-19 cases in hospitals are going up,” he wrote.
“They’re concerned about what happens if they or their kids contract the virus and they have to stay home with no pay if they’re out of sick time. They’re concerned about what happens if they lose even more staff to self-isolation requirements or illness, when many departments are already short-staffed and stretched thin. We saw these problems come up early in the pandemic, and here we are again.”
Boissonneault said Winnipeg Metropolitan’s current code orange provides an opportunity for everyone to help prevent a system overload.
“Wearing a mask may not be 100 per cent protection but its better than nothing and we need to do everything we can to flatten the curve.”
A spokesperson for the province said there are sufficient ICU beds in the system and extra capacity is available if needed. They said most ICUs have empty beds or patients on the transfer list.
"(Health Sciences Centre) Winnipeg, Manitoba’s provincial hospital, and other facilities with ICUs continue to provide care to critically ill patients from throughout Manitoba for a variety of issues, including COVID-19," they said. "The system also has the ability to repurpose resources to increase capacity as needed – including for those patients requiring ICU care."
They said the province has focussed on protecting staff who provide care to COVID and non-COVID patients, ordering more equipment including ventilators and beds in anticipation of surges, and ensure the necessary PPE is available.
They said the province's 'COVID-19 contingency planning' allows for more space, equipment and supplies to be purchased, and staff to be redeployed to areas that need more support.
"This could include the consideration of potential reduction of elective and non-urgent services like surgeries and diagnostic procedures in order to free up staff who could be redeployed," they said.
They said at this point the province does not anticipate shutting down areas of the health system in spring 2020.