WINNIPEG -- The pandemic has left Donna Becker with many questions, but one in particular is weighing on her mind—if she hadn’t put her husband in the Maples Long Term Care home in Winnipeg, would he still be alive today?
Donna Becker said she moved her husband Ted into the Maples in June 2019—it hadn’t been her first choice. She had tried to get her husband into the Middlechurch Home of Winnipeg—a publicly owned care home operated by the Winnipeg Regional Health Authority (WRHA)—but there was no room.
Becker said her 81-year-old husband—who lived with dementia—was taken to hospital in November where he tested positive for COVID-19, but was sent back to the Maples after one night. A week later on Nov. 25, 2020, Becker said her husband died.
"I know that I lost my best friend—the love of my life," Becker told CTV News.

Donna Becker (right) says her husband Ted (left) died on Nov. 25, 2020. Ted was one of 56 residents at the Maples Long Term Care Home in Winnipeg to die with COVID-19. (Submitted: Donna Becker)
Ted was one of 56 residents at the Maples to die with COVID-19.
The Middlechurch Home of Winnipeg has yet to report a COVID-19 case or death among a resident. Two cases were reported among staff.
"It is sad," Becker said. "Hardly anybody at Middlechurch got this, so you feel like you put him there—I put him in there."
At the time, Becker said she didn’t know the difference between Winnipeg’s non-profit, for-profit, and public care homes.
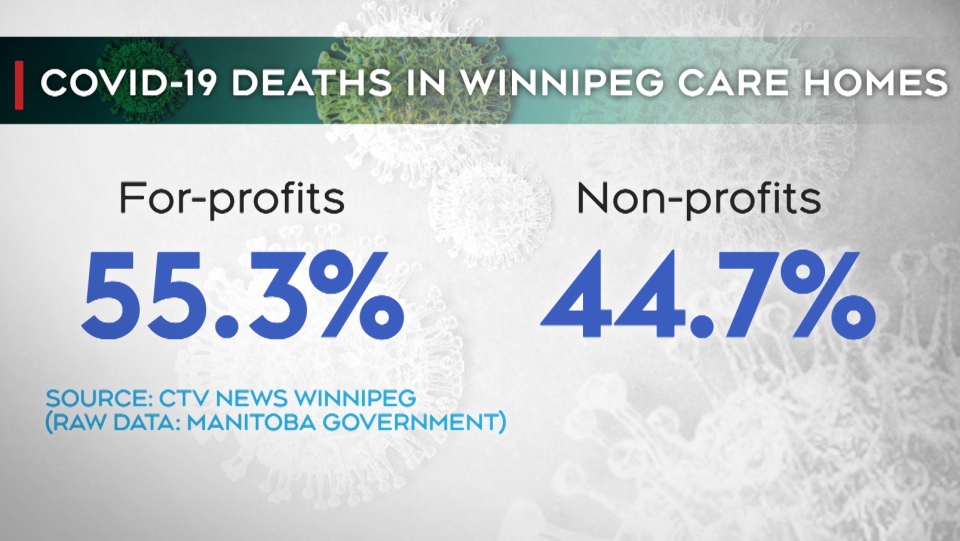
FOR-PROFIT CARE HOMES ACCOUNT FOR HALF OF WINNIPEG’S COVID-19 CARE HOME DEATHS
A CTV News analysis of the COVID-19 pandemic in personal care homes in Winnipeg between March 1, 2020, and March 2, 2021, found for-profit and non-profit care homes accounted for all COVID-19 deaths in care homes.
The data shows outbreaks have occurred so far in all but two of the city’s 38 care homes.
Of the total 351 deaths—more than half of them (55.3 per cent) were in for-profit care homes. The rest of the deaths (44.7 per cent) were in non-profit care homes.
Collectively, Winnipeg’s three publicly owned care homes, all of which are operated by the WRHA, had 14 cases and zero deaths.
The Maples—a for-profit care home run by Revera—is among Winnipeg’s deadliest COVID-19 care home outbreaks, with 231 total cases and 56 deaths. The 200-bed care home has a fatality rate of 28 per cent.
But it is not the deadliest care home outbreak in Winnipeg—a title held by the Charleswood Care Centre.
The 155-bed for-profit care home (also owned and operated by Revera) had 45 residents die due to COVID-19—leaving it with a fatality rate of 29 per cent. This is the highest fatality rate of any Winnipeg care home.
A WRHA spokesperson told CTV News a clinical lead has provided on-site support to the Charleswood Care Centre throughout its COVID-19 outbreak.
OWNERSHIP NOT A FACTOR IN COVID-19 OUTBREAKS, REVERA SAYS
Larry Roberts, Revera’s director of communications, told CTV News that advocates and observers have taken "ideological or political positions" when it comes to the ownership of care homes.
Roberts—in an emailed statement—said the level of community spread, and the age and configuration of a care home are significant variables in outbreaks, not ownership models.
"The pandemic hit the entire personal care home sector very hard; non-profit and publicly owned homes, as well as privately owned ones, experienced severe outbreaks," Roberts said, pointing to expert analysis.
"The extent of community spread is the key factor in assessing the cause of an outbreak and the age and design of the buildings was the most statistically significant factor in determining the severity of an outbreak."
He said while two Revera care homes were hit hard by the pandemic—topping the list of Winnipeg’s deadliest outbreaks in care homes—others, including its Kildonan care home, had no deaths and one case.
Within the Maples, Becker said she loved her husband’s nurses and was impressed with the home—but then the pandemic hit.
"I don’t know what happened. It wasn’t the nurses’ fault—it was Revera’s," Becker said. "They had plenty of time to plan for this, to get more staff in, to do something."
STAFFING AT A CRITICAL SHORTAGE BEFORE THE PANDEMIC: NURSES’ UNION
Following a deadly weekend at The Maples in November 2020, the province commissioned Dr. Lynn Stevenson to investigate the outbreak. Stevenson’s subsequent report outlined gaps in pandemic planning and a lack of urgency by Revera to call for help.
Among Stevenson’s recommendations is a call for the province to review care home funding to ensure they have adequate staffing levels.
Darlene Jackson, the president of the Manitoba Nurses’ Union, said the province was already in a critical nursing shortage before the pandemic hit.

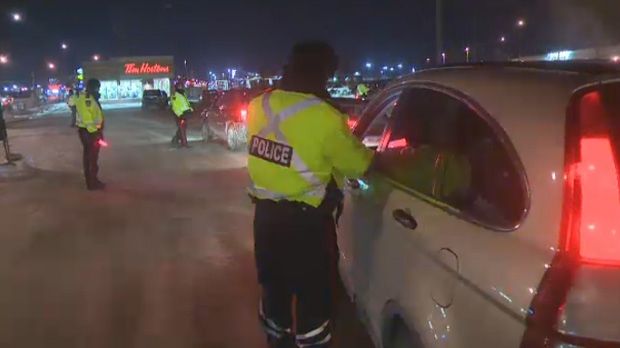
WFPS respond to multiple calls at the Maples Personal Care Home in Winnipeg during a deadly weekend in early November 2020. (Source: CTV News Winnipeg)
"Nurses are exhausted and riddled with grief from the loss of many of their residents, and patients they cared for, for years," Jackson said in a statement to CTV News.
Winnipeg-based epidemiologist Cynthia Carr said COVID-19 puts staff at high risk which can quickly leave the care home with a staffing shortage.
While staffing is a factor in outbreaks—Carr said it is not the only one.
HOW INFRASTRUCTURE PLAYS A PART IN CARE HOME OUTBREAKS
Not all for-profit and non-profit care homes were hit hard by the pandemic.
More than half of the 38 care homes in Winnipeg—both non-profit and for-profit homes alike—had three or fewer deaths connected to COVID-19.
Carr said COVID-19 outbreaks in care homes sometimes come down to the layout of care home buildings, which can put residents at risk.
"What care homes have in common is that people are in a communal living situation. They may have their own room, but in some settings they don’t," Carr said, adding if a visitor or staff member unknowingly brings the virus into that setting—it can spread quickly.
"A different home may have a different risk based on the layout of their facility."
It’s a problem that Brenda Hodgson, the acting CEO of the non-profit Convalescent Home of Winnipeg, saw firsthand.
The care home's current 84-bed building was built in the 1960s. It includes 15 shared rooms with four beds per room—a factor that played into what became a deadly outbreak.

Brenda Hodgson, the acting CEO of the non-profit Convalescent Home of Winnipeg, saw first hand how infrastructure played a role in a deadly COVID-19 outbreak. (Source: Josh Crabb/ CTV News Winnipeg)
The Convalescent Home of Winnipeg had an outbreak declared on Dec. 6, 2020. In a matter of days, Hodgson said cases spiked from three to more than 50.
"It’s showing that you need space—in the future, we need to build homes that are ready when there is a virus," Hodgson said.
"We have no space, we can’t social distance. We have multiple people in a room."
Hodgson said they had to treat everyone in the home as if they had COVID-19.
By the time the outbreak was declared over in February, the care home had reported 91 cases among staff and residents and 20 deaths—leaving it with a fatality rate of nearly 24 per cent, among the five highest in the city.
"I don’t think there is words to describe how hard it was, how (physically) exhausting and how mentally exhausting it was," Hodgson said. "There wasn’t a lot of time to grieve or even process."
MANITOBA DOES NOT TRACK CARE HOME OWNERSHIP IN PANDEMIC DATA
A spokesperson for the province told CTV News that public health does not document the ownership structure of care homes when tracking COVID-19 cases and deaths.
The spokesperson said the province’s COVID-19 data does not address how people in homes may have been exposed to the virus, nor how their pre-existing conditions and health status affected their risk of COVID-19.
They said the province plans to implement Stevenson’s recommendations in all personal care homes in Manitoba.
It’s a thought echoed by Manitoba Health Minister Heather Stefanson.
"We’ve seen the devastating impacts of the pandemic in private, non-for-profit and publicly owned long-term care facilities all across the country," Stefanson said in an email to CTV News.
"We’re focused on implementing the recommendations of Dr. Stevenson’s report to improve care for Manitobans not only at the Maples site, but at all personal care homes in the province, regardless of ownership."
METHODOLOGY
CTV News obtained COVID-19 personal care home data from the Province of Manitoba which accounted for all cases and deaths between March 1, 2020, and March 2, 2021.
CTV News calculated fatality rates based on the number of beds per facility.
The Province of Manitoba has not released COVID-19 data on the Extendicare Vista Park Lodge and Luther Home in Winnipeg. A provincial spokesperson said to date COVID-19 outbreaks have not been declared at the homes, and so it does not have information on COVID-19 deaths to report.