WINNIPEG -- Restricted access – the simple warning plastered on the doors of what used to be an orthopedic unit at the Health Sciences Centre in Winnipeg. Behind these doors is a 'COVID-19 Red Zone' where front-line workers care for some of the sickest and most infectious patients in the province.
Since the pandemic first hit Manitoba in March, nearly every unit in the Health Sciences Unit has been forced to make changes to deal with a surge of infectious patients.
CTV News has been given its first look inside one of Manitoba's 'COVID-19 Red Zones' and a glimpse at the pandemic's impact on the health-care system and those working on the front line.
INSIDE THE HEALTH SCIENCES CENTRE'S COVID-19 UNITS
Before patients showing symptoms of the virus get to the 'Red Zone,' they are screened for COVID-19 and wait in a specialized isolation area. The wait can sometimes last up to eight hours and can create a bottleneck in the emergency room as microbiologists work to complete the tests in a lab within the hospital.
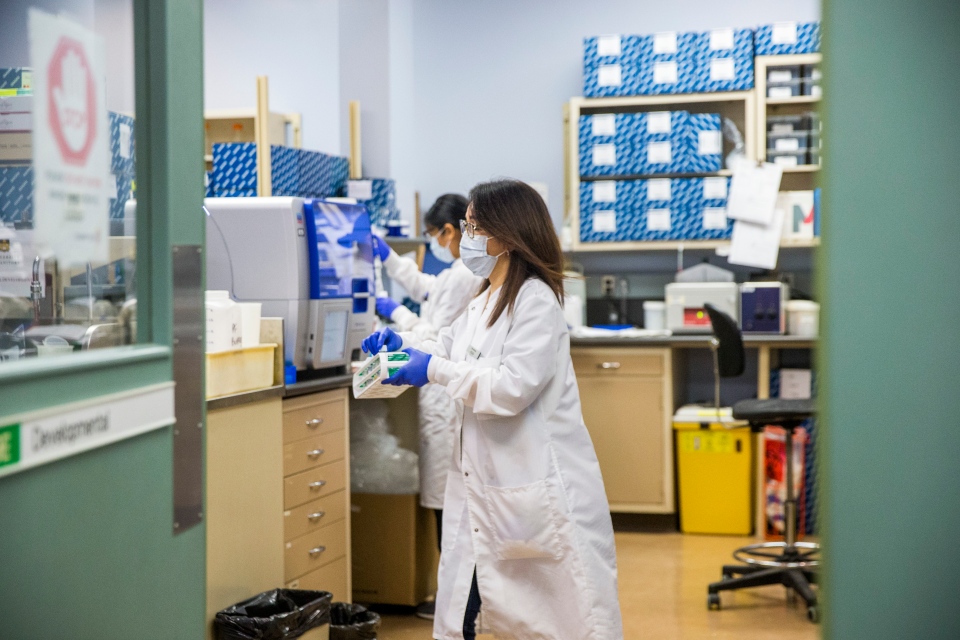 The microbiology lab at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
The microbiology lab at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
The pandemic has essentially doubled their workload.
"There's been some talk that emergency departments don't look that busy, but I assure you, it feels like we're very busy," said Dr. Shelly Zubert, the assistant director of the HSC emergency department.
Within the department is a trauma room, where patients needing resuscitation are brought in. It starts with a call from Emergency Medical Services bringing the patient in. Zubert said the emergency room teams have 30 seconds to get dressed in full personal protective equipment (PPE) and prepare for the incoming patient.
"With the community spread and the positivity rate in our community, we have to assume a lot of those patients coming in have COVID exposures in the community," she said.
"Every time those patients come in, there's a heightened sense of importance to receiving those patients in a safe manner."
 The adult emergency department at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
The adult emergency department at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
Patients are moved from the ER to different COVID-19 units – some units have plastic curtains to create a protective barrier around the patient, others have full cubicles for each incoming patient.
'EVERYTHING'S CHANGED': HEALTH-CARE STAFF FACE BIG LEARNING CURVES
Anna Marie Papiz, the manager of a 30-bed orthopedic unit at HSC that has been converted to a Red Zone, said the shift has been a big learning curve for staff.
"Working on a red zone area is much different than working on a normal medicine or surgical unit," she said.
Even the mundane tasks, like sending dirty laundry to the wash or taking out the garbage, have become more difficult. Staff entering these units must wear PPE and are required to leave personal items outside.
"Everything's changed for them and it has been difficult, but this unit has been a huge support for one another."
Papiz's unit is just one of six at HSC that has been converted to manage COVID-19 patients. There are eight more COVID-19 units in hospitals across the Winnipeg health region, as well as one in the Prairie Mountain Health Region and one in the Southern Health region.
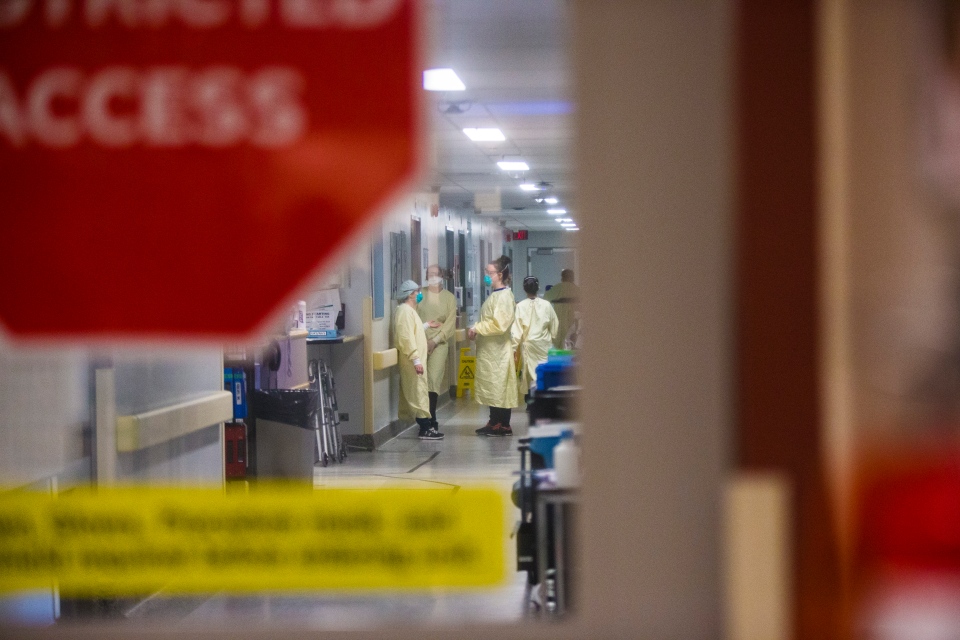 A COVID-19 unit (which used to be an orthopaedic surgery unit) at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
A COVID-19 unit (which used to be an orthopaedic surgery unit) at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
While these health-care workers deal with the virus up close every day, Papiz said leaving that 'Red Zone' can cause anxiety.
"They know these patients are COVID-positive patients, and they can wear all that extra PPE," she said. "The piece that frightens them more is going outside of these areas, and outside of even the walls of this facility, where we don't know who might be carrying that virus."
Inside the HSC medical intensive care unit - all 20 beds are usually full, with both COVID-positive and negative patients.
IN PICTURES: Red Zone: On the frontline of Manitoba's COVID-19 pandemic
Dr. Bojan Paunovic, the site director for HSC's critical care, said staff at four different hospitals are managing 120 critical care beds.
"That's over 150 per cent capacity, that's a level that we as a health-care system, we're probably expected to achieve in order to deal with this, but it's not a level that is indefinitely sustainable," he said.
Not only are staff caring for more patients, but they are also faced with a bigger workload – constantly monitoring and evaluating patients to see if they're ready to be transferred to a less acute area, and make room for others to be admitted.
"Long-term in order to support this, other parts of the system have had to come help."
HEALTHY MANITOBANS PAYING PRICE FOR STRAINED HEALTH-CARE SYSTEM
Paunovic said the redeployment of these staff means other parts of the health-care system are not delivering the care the way it should be – which is why many operating rooms at HSC sit empty.
While the daily tasks of health-care staff have changed, their job remains the same – keep people alive. Dr. Edward Buchel, the head of surgeries at HSC, said that is coming at a cost healthy Manitobans are paying.
 An operating room in the empty day surgery unit at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
An operating room in the empty day surgery unit at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
More COVID-19 patients admitted to hospitals means more beds are required to care for them.
"We need staff with those beds. We need human beings to keep care of other human beings," Buchel said.
A large portion of that staff is available because the province is cancelling elective and non-urgent surgeries. Buchel said the number of surgeries has been cut in half in Manitoba.
"We're using the resources that would normally go to those people, to maintain our COVID positive patients in our hospital," Buchel said.
While urgent surgeries are going ahead – these include surgeries for limbs, life-threatening injuries, traumas, and cancer – what Buchel called "quality-of-life" surgeries are being cancelled.
Younger Manitobans may not be at high-risk for severe outcomes from the virus, but Buchel said if they, for example, blow out a knee while skiing or skating and need surgery – they will be out of luck.
 Dr. Ed Buchel, provincial specialty lead of surgery, walks through the empty hallways in the day surgery unit at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
Dr. Ed Buchel, provincial specialty lead of surgery, walks through the empty hallways in the day surgery unit at the Health Sciences Centre in Winnipeg on Tuesday, Dec. 8, 2020. (MIKAELA MACKENZIE / WINNIPEG FREE PRESS)
"You need your ACL repaired, you have a hip that needs replacement, or you have a breast cancer that needs reconstruction; those are gone," he said.
"We're not doing those. We're doing anything that needs to be done to keep you alive, to keep your limbs on."
THOUSANDS OF SURGERIES CANCELLED AMID PANDEMIC
Shared Health said about 5,300 surgeries were cancelled or postponed during the first wave of the pandemic in Manitoba, causing a backlog in surgeries that was still being cleared when the second wave of the pandemic hit.
An estimated 2,750 surgeries have been cancelled or postponed since a surgical slowdown was initiated on Oct. 26.
For the Manitobans who have had a surgery cancelled – they may be given some drugs to help manage the pain while they wait.
Shared Health said if health-care workers believe a prolonged delay in surgery will have a negative long-term effect on a person’s health, their surgery will be scheduled.
Buchel said the health-care system checks in on these people to make sure they are not getting sicker.
"We keep on waiting, we keep on watching, and we adjust."
This is part one of a three-part series 'Red Zone: On the frontline of Manitoba's COVID-19 pandemic' from CTV News giving Manitobans a deeper look at the impacts of the COVID-19 pandemic on our health-care system.
Part two of this series will be released on Dec. 18, showing the impact COVID-19 has had on end-of-life care and a family's final goodbye in a pandemic.