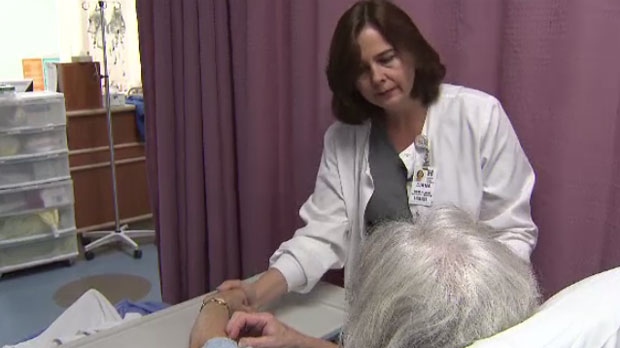
It's the cost of caring, and Manitoba helpers are paying the price.
Compassion fatigue is now recognized as a key concern to the mental and emotional well-being of caregivers, that has profound effects on workplaces and communities.
"Compassion fatigue refers to this emotional and physical erosion that helping professionals and family caregivers can experience when they're being thrust into situations where they have to continually give and give of themselves,” said Francoise Mathieu, who specializes in working with organizations across North America to address the issue.
Mathieu said while it’s unclear whether instances are increasing or awareness is heightened, compassion fatigue has become a growing concern in the helping professions over the past five years.
“You either numb out, or become less sympathetic over time,” said Mathieu.
She said loved ones are often the first to notice warning signs and suggests asking the affected caregiver what a hard or difficult day looks like for them, and what they need in order to self-care.
Caregiver Cathy Hurd Carter said at first, it was difficult to admit she was the one who needed help.
"I felt like I was going to fall apart. I felt like I had hit that proverbial brick wall,” she said. “It was like there was no way out, I was in a pit and I had no way to climb out."
A career caregiver in the community, Hurd Carter was thrust into helping her husband Tom, nicknamed ‘Bos’, after he sustained a severe work injury in 2011. Shortly after, he was diagnosed with dementia.
Now caring for him full-time, Hurd Carter continued to ignore her signs of compassion fatigue until it reached a crisis point.
"We are often the ones people turn to for help, but when the caregiver burns out, where do we go?” said Hurd Carter.
All people working in helping professions are at risk of compassion fatigue.
Sandi Mowat, the president of the Manitoba Nurses Union, said the condition is a growing concern for nurses.
A recent study of MNU members found 62 per cent of Manitoba nurses currently experience compassion fatigue, while 71 per cent have experienced burn out at some point in their career.
The MNU is lobbying the province for more support.
Mowat said work overload, combined with the stigma of seeking help as a caregiver, are barriers to treatment.
“Currently there are some supports, but it’s hit and miss,” said Mowat. “We want it to be something that is mandatory, that's offered to nurses on a regular basis, particularly when they're involved in a critical incident or traumatic event.”
United Fire Fighters of Winnipeg has also focused attention on the mental well-being of its members.
Legislation is in the works with the Workers Compensation Board to improve supports.
Alex Forrest, UFFW president, said the first thing is to create a safe place for fire fighters to come forward and admit they have issues. The union is also working to train officers to spot the outward signs of compassion fatigue in team members before it escalates.
"Many times these issues translate into such things as substance abuse, anger management, divorces, social reality issues, mental health issues," said Forrest.
Untreated compassion fatigue can develop into post-traumatic stress disorder, which can lead to tragic consequences.
The condition is inflamed by diminished resources, work overload and the burn out of fellow colleagues.
Specialist Francoise Matheiu said those who feel the fatigue, which can ebb and flow over the course of a career, are people who excel at their work.
She said compassion fatigue should be a concern for everyone because over time, services are losing helping professionals who end up on stress leave – or worse.
A provincial inquest into the death of Brian Sinclair -- a Manitoba man who died in an ER waiting room after being left unattended for 34 hours -- notes compassion fatigue as a contributing factor to the incident.
The inquest recommended regional health authorities look into the feasibility of incorporating more training in the emotional safety of its workers.
So far, the Winnipeg Regional Health Authority has implemented an annual staff engagement survey to determine what needs to address; such as increasing the amount of recognition given to staff on a daily basis.
“Getting that positive feedback can really help the person to build some of that resiliency they need so that the issues relating to compassion fatigue may not be able to take root," said Lori Lamont, Chief Nursing Officer with the WRHA.
CTV also reached out to Winnipeg police to find out how the service addresses mental health.
“The Behavioral Health Unit (BHU) is in place to address any difficulties a member may face,” said Const. Eric Hofley, WPS, via email. “The unit consists of a psychologist, two full-time and three part-time wellness officers. As well, there is a Peer Assistance Program.”
In a critical incident, involved members are provided with immediate counseling and any follow-up counseling if required.
A police officer can contact the unit at any time if they need.
As well, Hofley said the service encourages all members to be aware of co-workers who may be struggling, support them as necessary and encourage them to seek help.
Public help is offered through Addictions Foundation Manitoba, who recommends using this online resource for more information.